A 61-year old male patient came to the ER of KD Hospital with a complaint of left-side chest & shoulder pain since half an hour. Investigative ECG showed ST Elevation from V1-V3 indicating Anteroseptal Myocardial infarction & the 2D Echo showed LVEF (Left ventricular ejection fraction) of 10-15%. An ejection fraction below 40 % indicates a failing heart.
Suddenly, the patient went into cardiac arrest in the ER itself. The medical team under the guidance of Dr Vivek Nanda, Consultant Emergency Medicine, rushed to revive the patient with the help of continuous CPR and shock (electrical cardioversion), by 360J unsynchronized current. With electrical cardioversion, a high-energy shock is sent to the heart to reset a normal rhythm.
Later, the return of spontaneous circulation (ROSC) was achieved & the patient was then admitted under the care of Dr Abhishek Rajpopat, Consultant Cardiology for further management. A Coronary angiography diagnosed the patient with Acute coronary syndrome, Double vessel disease, Acute anterior wall myocardial infarction, Cardiogenic shock & Severe LV dysfunction.
Understanding the urgency & delicate condition of the patient, the Cardiologist performed Percutaneous transluminal coronary Angioplasty (PTCA) in the left anterior descending artery (LAD) on intra-aortic balloon pump (IABP) support.
An intra-aortic balloon pump (IABP) is a type of therapeutic device, that helps the heart pump more blood. IABP therapy is used to treat Cardiogenic shock.
Later the patient was stabilised in the ICU and was sent home walking after a stay of just 5 days.
A 59-year-old uncontrolled diabetic & morbidly obese patient was referred to KD Hospital in a hypoxic state on maximum ventilatory support - for consideration of ECMO following severe pneumonia secondary to H1N1 influenza (Swine Flu) infection. Based on her critical situation, she was admitted under the care of Dr Harjitsingh Dumra (Consultant Pulmonary & Critical Care) & Dr Mansi Dandnaih (Consultant Critical care and Liver Transplant Intensivist).




Weighing the risks/benefits involved with ECMO (An advanced technique to improve oxygen in patients failing ventilator support), a decision was made to give her a trial of prone positioning ventilation (patient lying flat on the stomach) to facilitate oxygenation. She required two sessions in the first 3 days (for 18 hours/day). It was challenging to glue Prone Ventilation in this case as she was morbidly obese (104 hg Bodyweight) e having acute kidney Injury (Creatinine: 3.40 mg/dL). The experience and skill of the treating team made this herculean task possible. Under the continued supervision of the ICU staff and timely decisions relating to appropriate antibiotic, fluid, hemodynamics and ventilator therapy, the patient eventually made a complete recovery.The patient required 14 days of ventilatory care, 20 days of ICU & total of 27 days of Hospital stay.
This monumental task was only possible because of seamless coordination between different specialties involved & implementation of state of the art protocols. The painstaking & untiring efforts of the entire ICU Team not only led to the survival of the patient but also led to avoidance of ECMO, which would have added a substantial burden to the cost of therapy. This was surely a Miracles of Care !
A 40-year male patient visited KD Hospital's Department of Orthopaedics with a complaint of pain in the left knee for 15 years, debilitating his life. Upon consultation with Dr Amir Sanghavi and undergoing a diagnostic X-ray, he was found to suffer from Left Knee Osteoarthritis with fixed flexion deformity of 25 degrees.


After thorough counselling and weighing the benefits of surgical intervention, the patient underwent left-side Robotic Knee replacement surgery, which involves resurfacing a knee damaged by arthritis. Robotic surgery helped in perfect alignment and ensured the longevity of the implant. After surgery, he returned home pain-free & stable.
The uniqueness of this case reflects in the fact that for a better quality of life, the patient underwent Knee surgery at a relatively younger age. Due to several myths surrounding knee replacement surgery, the patient did not consult a specialist at an early stage. If he had consulted sooner, he would have suffered less pain & have not lost several years to reduced mobility.
A 35-years old female patient, known case of gestational diabetes mellitus, came to KD hospital. She was 37 weeks pregnant, with fever, extreme weakness and reduced fetal movements. Her blood work showed Dengue positive status, severely low platelets (15,000/mm3) & elevated liver enzymes. Additionally, baby's heartbeat tracing showed Fetal distress.
It was a situation of distress because she needed emergency delivery by Caesarean to save the baby. But any major surgery with such low platelets is very high risk for the mother as she may bleed profusely. ICU admission platelet transfusions were given & emergency Caesarean was done by Dr Ankita Jain (Consultant Obstetrician and Gynaecologist). Postoperatively she received more platelet & blood transfusions & was stabilized in ICU.
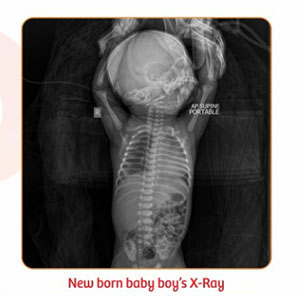
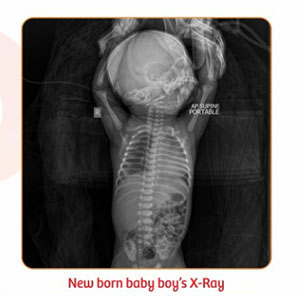
A baby boy was then delivered & admitted in NICU under the care of Dr Snehal Patel, Consultant Neonatal Paediatric Intensivist due to Respiratory distress as result of MSAF (Meconium stained amniotic fluid) & dengue positive status of mother. Baby's platelets were 9000/mm3 on admission e- dengue viral load was very high. The Respiratory distress settled within next 2-3 days with supportive care, but his platelets were breaking down and required multiple transfusions. The baby also had low BP & reduced cardiac output which was managed aggressively with fluid & ionotropic support. He showed signs of Liver failure due to dengue hepatopathy as well. Gradually with proper intensive care, his liver enzymes & platelets improved & finally the mother was involved for feeding the baby.
Both mother & baby were discharged in stable condition due to the promptness & expertise of our expert Doctors.
A 49-year old male patient with incidental detection of large left adrenal mass, came to KD hospital, Ahmedabad. Based on his condition & history of presenting illness he was admitted under the care of Dr Darshan Shah, Consultant Urologist Dr Darshil Shah, Consultant Urologist.
He was suffering from transient ischemic attack (TIA) headache, which is a temporary period of symptoms similar to those of a stroke. Upon investigation it was found that the patient had Left Adrenal Myelolipoma. Depending on investigative reports & after weighing the treatment options, the Urologists decided on excising the adrenal mass.
He was treated with Laparoscopic left adrenalectomy & an adrenal mass of site 10 x 9 cm approx. was removed.
Laparoscopic Adrenalectomy (LA) is a minimally invasive surgical approach that has almost replaced the open adrenalectomy in the management of small and medium-sized adrenal lesions. The patient was then relieved of his severe symptoms & was discharged in a stable condition.
The advantages of Laparoscopic adrenalectomy in such cases include shorter hospital stays, decreased postoperative pain, improved recovery times, and better cosmetic results.
A 24 year old female patient presented in the Emergency room with complaints of severe headache and blurring of vision. She was referred to the Ophthalmology Department for a Fundus examination as the patient revealed history of chronic intermittent headache. On examination her vision in both eyes had decreased significantly - she was able to see objects only from a very close range. Both eyes had conjunctival congestion with comeal edema. The Anterior chamber was flat with a complete iris-corneal touch. Her Pupils were 6 mm dilated and were sluggishly reacting to light. Intraocular pressure was measured to be 62mm Hg and 64mmHg in right and left eyes respectively.
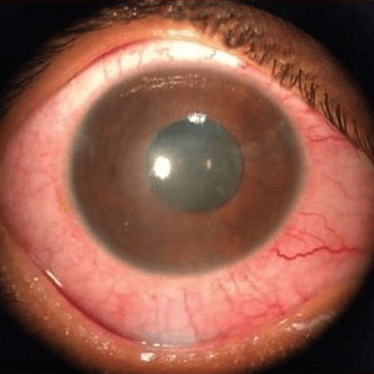

The images show both eyes having severe redness and edema on her corneas with dilated pupils
A clinical diagnosis of Acute Angle Closure Attack was made based on the findings. On eliciting drug history, it was found that the patient was taking Topiramate for the headache, as advised elsewhere. She then underwent Laser Peripheral Iridotomy and has been improving significantly since then. Her vision and IOP have been recovered to normal levels.
Drug induced Glaucoma is a sight threatening idiosyncratic reaction which can happen from even a single dose of the triggering drug especially a Sulpha group drug. All patients who need to be put on sulpha based drugs such as Topiramate, need to undergo a thorough eye check up and must be advised regarding the symptoms of an angle closure attack.
A 24-year old female patient came to KD Hospital with complaint of sudden onset fluid discharge from the left-side of nostril. The patient was advised to undergo specific tests for a proper diagnosis. Her CT scan indicated of a Cerebrospinal fluid leak and she was then diagnosed with CSF rhinorrhoea.
Cerebrospinal fluid (CSF) is a watery liquid that continually circulates through the brain's ventricles (hollow cavities) and around the surface of the brain and spinal cord.
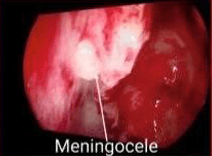
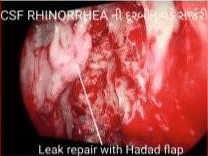
A CSF leak can cause fluid to leak through the ears, through the nose or into the spinal canal. It must be diagnosed and treated efficiently to prevent meningitis, an infection of the meninges.
For her treatment, the patient was then admitted under the care of Dr Hardik Shah, Consultant ENT. After weighing all existing options, both invasive and non-invasive, a decision was made to perform Endoscopic CSF leak repair under general anaesthesia.
Endoscopic repair of CSF rhinorrhoea is safe and effective, with a very low complication rate. It has almost completely replaced the older open techniques.
After surgery the patient was kept under observation & treated with IV fluids, IV antibiotics and other supportive medications. Due to the prompt response of the ENT expert e his swift decision making, the patient was discharged within 5 days of admission in a stable condition, free of any symptoms.
This case shows the importance of adapting to newer e non-invasive techniques when it comes to surgical treatment. The benefit is that this technique is scarless, reduces hospital stay e cost, while giving better outcome. Every nasal discharge is not common cold & the possibility of a CSF leak should never be ignored.
A 17 year old boy from Bikaner was successfully operated for a severe spine condition at KD Hospital, Ahmedabad. Shyam kumar (name changed) was suffering from Scoliosis or abnormal curvature of the spine since last 4 years, due to which he was in severe pain e discomfort. Not only it was a significant cosmetic issue for him but was also causing him difficulties in doing day-to-day activities.


Scoliosis surgery can be very risky, and there is a chance of paralysis as well. Patients are often afraid of getting surgery due to the high risk, however, they were informed about the new technology available with KD Hospital which has improved surgical outcomes associated with it.
"The entire surgery was done under advanced technology like Neuromonitoring & Spinal Navigation and was completed within 4-5 hours. After the surgery, his spine has become straighter as compared to before e the pain has also reduced significantly. He was able to stand and walk after surgery on the second day itself and Having recovered from his illness, he is currently living an active normal life with confidence." explained Dr Hrutuij Bhatt, Consultant Spine Surgeon at KD Hospital, Ahmedabad.
A 39-year old morbidly obese patient (weight 255 kg) came to KD Hospital with complaints of breathlessness during walking, hypertension e disturbed sleep pattern since several years. His obesity had a severely ill effect on his overall life quality & was gradually becoming a significant reason for his depression. With a habit of drinking approx. 8L of Soft drinks per day, he had a poor quality of life e was on regular medications. Upon admission, his weight was 255.5 kg e BMI was 91.5 Kg/m2.
His USG abdomen showed moderate to gross hepatomegaly with prominent fatty changes along with significant Gallbladder calculi.

He was advised to undergo a Laparoscopic Gastric bypass by Dr Manish Khaitan, Senior Bariatric Surgeon. Laparoscopic gastric bypass (GBP) surgery is a procedure that involves the creation of a gastric pouch surgically and performed to yield significant and long-lasting weight loss in patients who are severely obese.
Regular check-ups, dietary changes and lifestyle modifications made up a significant part of the patient's post-operative journey. Follow-up visits at regular intervals with constant medical e psychological support were instrumental in this patient's weight loss journey. One year after undergoing life-changing bariatric surgery, the patient currently weighs 149 kg e aims to lose even more weight.
A 42-year-old patient suffered from recurrent episodes of altered senses, jaundice, and fluid accumulation in the abdomen since 10 years. On evaluation, he was found to be suffering from liver cirrhosis. He worked for the City's Police department but due to disease-related complications, he was unable to perform the job efficiently. As a permanent cure, he was advised Liver Transplantation at KD hospital by Dr Divakar Jain, Consultant Liver Transplant & HPB Surgeon. As a Liver Donor, the patient's wife came forward to help.

Intraoperatively, his hugely dilated portal vein was a big challenge. The challenge was in joining the 3 cm dilated recipient portal vein with the 8 mm sized donor portal vein. Also, there were hugely dilated veins under the skin and inside the abdomen. The technical problem was dealt with efficiently by the experienced Liver transplant team. The patient and donor, both were stable at the time of discharge
Liver Transplantation is a complex surgery and requires a skilled and experienced team for a consistently successful outcome. In such cases, the benefit of Living-Donor Liver Transplant is absence of waiting period.
A 64-year-old patient came to the Neurosciences Department of KD hospital with a complaint of disturbed sleep for 7 years. He reported waking up 2-3 hours after falling asleep due to tingling and numbness in his left hand and arm. Despite trying multiple medications, he had not found significant relief.
Upon consultation with Dr Rutul Shah, it was determined that the patient was likely experiencing dynamic nerve compression near his elbow while sleeping. This was causing decreased blood supply to the nerve and resulting in symptoms.


In order to reach a confirmed diagnosis, the patient underwent a Nerve conduction study and Ultrasonography of the nerve. The Nerve conduction study was done to identify which nerve was affected and the extent of nerve damage, whereas the Ultrasonography was done to directly visualize the site and extent of ulnar nerve damage.
The patient was finally diagnosed with Ulnar nerve damage at the elbow. He was treated with an elbow brace to be worn at night. After one month of treatment, the patient reported significant improvement and declared "Doctor, I finally had a good night's sleep after 7 years!!"
A 23-year old young female patient came to KD Hospital, Ahmedabad with complaints of swollen feet, dyspnoea on exertion and vomiting since last 6 months. On investigation, her Serum Creatinine was found to be 6 mg/dL which was instrumental in diagnosing her with ANCA-associated Renal Vasculitis by Dr Kamal Goplani, Consultant Nephrologist, KD Hospital.
ANCA vasculitis is an autoimmune disease affecting small blood vessels in the body. It is caused by autoantibodies called ANCAS, or Anti-Neutrophilic Cytoplasmic Autoantibodies. Kidney involvement is very common in ANCA- associated vasculitis.
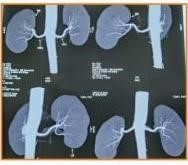
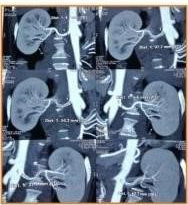
Due to this, the patient was initiated on maintenance Haemodialysis but it didn't improve her condition. After weighing all available treatment options e understanding the urgency of the situation, the patient & her family members were explained regarding the need for a Kidney Transplant. The patient's mother came forward as a Kidney Donor due to matching blood group.
A Kidney Transplant was then performed successfully and induction with Tacrolimusin Tacrolimus, and Mycophenolate Mofetil was done. On the 4th post-operative Day, her condition significantly improved & her creatinine was reported at 0.8 mg/dL with a urine output of 3L. The patient & the donor were then discharged in stable condition.
A 60-year old female patient from Tanzania came to KD hospital with a complaint of Pain in both hips and difficulty in walking e sitting since 2 years. Since then, she had been looking for a solution to her long-standing problem but was unable to do so.
Upon her arrival at the hospital, she consulted Dr Ateet Sharma, Senior Robotic Joint Replacement Surgeon and was advised for an X-ray of Pelvis with both hips. Based on the X-ray, she was diagnosed with Bilateral Hip osteoarthritis. Hip osteoarthritis is the deterioration of the cartilage of the hip joint and one of the causes for this is age-related wear and tear.


After thorough counselling es weighing the benefits of Surgical intervention, the patient underwent surgery of Replacement of both hip joints. In a Total hip replacement, the surgeon removes the damaged sections of the hip joint and replaces them with artificial implants that are biocompatible. This artificial joint helps reduce pain and improve function.
Post surgery, the patient recovered well with help of medications e physiotherapy sessions e was immensely satisfied with the exceptional care that she received. With a smooth recovery, she got back on her feet & was able to walk without pain.
A 50-year old female patient was brought to the ER of KD Hospital, Ahmedabad at early morning hours with complaint of sudden onset breathing difficulty, profused sweating e syncope, since half an hour. On arrival, patient was dyspneic with an elevated Respiratory rate of 30/min, Heart robe of 120/min and BP of 70/50 mmHg. Her ECG showed sinus Tachycardia with NO ST-T changes. As a part of her initial assessment in the ER, a POC USG was performed which suggested Normal EF (Ejection Fraction), No RWMA (regional wall motion abnormalities), Right Atrium/Right Ventricular Dilatation, IVC (Inferior Vena caua) Dilatatione No Pericardial Fluid.
The findings were suggestive of Acute massive Pulmonary Embolism (PE). The Wells's score for Pulmonary Emboli was 4.5 for this patient. The Wells criteria for pulmonary embolism is a risk stratification score and clinical decision rule to estimate the probability for acute pulmonary embolism (PE) in patients with a diagnostic possibility. Based on these findings. a CT Pulmonary angiography was immediately performed. Filing defects at multiple levels on Bilateral pulmonary arteries were seen, which helped in the final diagnosis of Acute massive Pulmonary Embolism, as confirmed by Dr Vivek Ambalio, ER consultant.


Dr Krunal Tamakuwala, Interventional Cardiologist immediately took a decision to performed Thrombolysis with Tenecteplase. Thrombolytic therapy is used in patients with acute pulmonary embolism (PE) to rapidly dissolve the embolic burden and improve cardiorespiratory hemodynamics. After Thrombolysis, the patient symptomatically improved, with a stabilized BP & the ECHO also showed regression in RA/RV within 2 hours time. The Patient was then discharged after 2 days in a hoemodynamically stable condition. Pulmonary Embolism (PE) is the condition in which blood clots are stuck at one or multiple locations in the blood circulations of the lungs- compromising the Oxygenation of blood. Eventually causing obstructive shock. If not diagnosed or treated in time, it becomes a life threatening condition.
A 25 year old young male patient, suffering from Malaria was brought to the ER of KD Hospital, with severe breathing difficulty. Due to prolonged illness, the patient developed Acute respiratory distress syndrome (ARDS), a life-threatening lung injury that allows fluid to leak into the lungs. During treatment, the Doctors closely monitored him due to his critical condition. To facilitate breathing, he was provided Prone ventilation (patient lying on their abdomen in a monitored setting, requiring a ventilator). With a holistic approach of physiotherapy, mobilization with a ventilator, antibiotics & good nutrition, he recovered & was discharged in a stable condition after 21 days of stay.

The uniqueness of this case reflects in the fact that the treating Doctors were able to prevent Severe secondary infection & revive the patient even with slow recovery.
A 64-year old female patient visited KD Hospital's Department of Orthopaedics with a complaint of left shoulder pain & difficulty in movement since 6 months. Due to immense pain in the shoulder region, the patient couldn't carry out any regular tasks or perform basic functions.
Upon Consultation with Dr Chirag Patel, Senior Consultant Joint replacement surgeon e undergoing a diagnostic Shoulder X-ray, she was found to be suffering from Shoulder Osteoarthritis. Shoulder arthritis occurs when the cartilage starts wearing down on the ball and/or socket sides of the shoulder joint. Symptoms of shoulder arthritis usually include pain in the shoulder joint, stiffness and reduced range of motion.


A Reverse Shoulder Arthroplasty was then recommended to the patient. A reverse prosthesis is designed for situations where the rotator cuff is torn or malfunctioning. l.e, irreparable rotator cuff arthropathies.
After a successful surgery, for recovery the patient was advised specific rehabilitative exercises. Additionally, by utilizing a holistic approach, including adequate exercises, proper nutrition & medication, she was able to return home pain-free e stable. Reverse Shoulder replacement is a treatment option for those that would not benefit from traditional shoulder replacement. A reverse replacement may be indicated in those with rotator cuff tears and arthritis, traditional shoulder replacement failure, or consistent dislocations of the shoulder.
A 6-year old boy was brought to KD Hospital, Ahmedabad by his parents with complaints of persistent cough since 6 months. He had no complaints of Dyspnoea, wheezing or fever. His parents previously consulted with several other doctors but he did not get any relief from the medications. Upon arrival at the Pulmonary & Critical Care Department of KD hospital, he was examined by Dr Pradip Dabhi, Interventional Pulmonologist & Lung Transplant Physician.
The patient underwent investigation in the form of CT Thorax which showed foreign body impaction in the right intermediate bronchus. It provides detailed visualization of the lung parenchyma and is used to evaluate chronic interstitial lung disease or any form of obstruction to the airflow.

Understanding the urgency of the situation and weighing all the existing option, a decision was taken by the Doctor to perform a Bronchoscopy & remove the foreign object. Bronchoscopy is a minimally invasive procedure that lets the doctor take an in-depth look at the airways and lungs. In this case, Flexible bronchoscopy was used to diagnose and remove foreign bodies. Flexible bronchoscopy is more convenient as patients are only lightly sedated with a high success rate (90%).
After Bronchoscopy, a small piece of Betel nut was removed from the young boy's lungs. The patient was then kept under observation and was discharged in a stable condition on the same day. This case highlights the importance of Non-inuasive techniques as opposed to surgical procedures, in case of treatment for children.
An 11 year old boy was brought to the Emergency room of KD Hospital by his parents, in absolute panic situation. He was having continuous blood uomite passing bloody stool along with severe abdominal pain. His blood pressure e 02 saturation on arrival was also very low.
The patient's father was given a guarded prognosis by referring doctors outside KD Hospital, as the young boy was having persistent blood loss. Upon consultation, it was found that his condition was deteriorating rapidly e he needed urgent treatment, hence he was admitted to the PICU under the care of Dr Snehal Patel, Consultant Paediatricse Neonatology. He was immediately started on treatment with IV fluids, 02 e medications to maintain his blood pressure.



His blood investigations showed Haemoglobin levels of 5 mg/dl, hence he was also given 2 units of blood in emergency. The reason why he was bleeding profusely was not clear. There was also a history of fever since 2 days. Further detailed investigations showed that he had Thrombocytopenia e was positive for Dengue PCR. Therefore blood products were given accordingly to treat this condition.
A cross reference was done with Dr Kartik Desai (Consultant Gastroenterologist) for further treatment. An Ulcer in stomach of - 2 cm size with spurting blood vessel was found & through Endoscopy therapy it was stopped. The most likely cause of an Ulcer bleed was NSIDS along with low platelets due to Dengue. These type of ulcer bleeds have 21% mortality rate and rebleeding rate of 34% in 1 week. The patient recovered without rebleeding e was discharged in a stable condition.
Gastrointestinal (GI) bleeding is one of the most life- threatening events in childhood. Bleeding may occur anywhere in the gastrointestinal tract and may be difficult to determine its location. Gl bleeding that originated from the esophagus, stomach, and duodenum can be characterized by hematemesis. In such cases, prompt identification e treatment is necessary as it's a life threatening event.
A 37-year old female patient from Kenya came to KD Hospital with complaints of heavy periods since 1 year e inability to conceive, since 2-3 years. She had been suffering from Gynaecology-related complications & was looking for expert treatment since a long time. It was at KD hospital, that she received the most accurate diagnosis.
Upon investigations, her USG showed multiple intramural and subserosal fibroids. Other diagnostic tests showed Right cornual block & Left distal hydrosalpinx. Her USG Surgically Removed Fibroids Pelvis showed a bulky uterus with multiple fibroids. After in-depth consultation, the patient was admitted under the care of Dr Ankita Jain, Consultant Gynaecologist. After all necessary scans and tests, a careful decision was taken by the expert Gynaecologist to operate and provide treatment surgically. The patient underwent Laparoscopic myomectomy & Chromopertubation, as part of her treatment plan.

Gynaecological Laparoscopy is a minimally invasive procedure that allows doctors to view the pelvic and abdominal cavities. When laparoscopy is performed for diagnostic or therapeutic purposes in women with infertility, chromopertubation (instillation of dye through the fallopian tubes) is performed to check whether the fallopian tubes are open. Myomectomy is a surgical procedure to remove uterine fibroids (which was one of the most prominent issue in this patient's case).
With great precision, the Gynaecologist was able to expertly perform the surgery e remove 9 fibroids of various sizes (2cm to 8 cm) from the patient's uterus. This played a key role in relieving the patient of her long standing issues. After recovery, the patient was discharged in a stable condition.