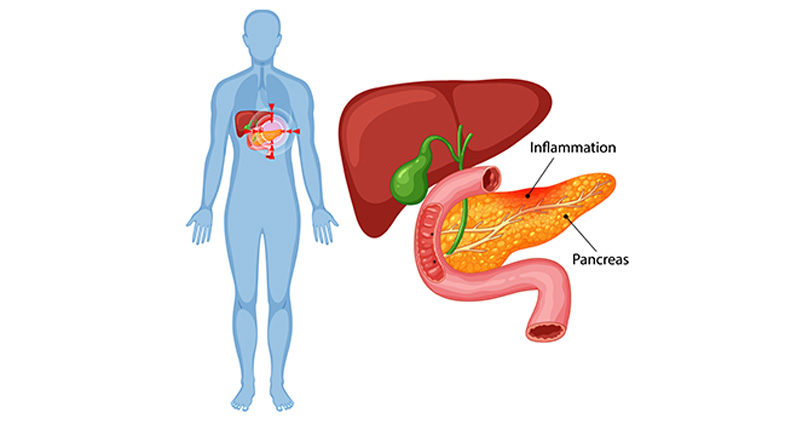
Chronic pancreatitis is a progressive inflammatory condition that can significantly affect a person’s quality of life. Over time, persistent inflammation causes irreversible damage to the pancreas, leading to chronic pain, digestive issues, weight loss, and even diabetes. Many patients manage the condition with lifestyle changes, medications, and enzyme supplements, but in case of unmanageable pain or complications, surgery may become necessary.
What is chronic pancreatitis?
Chronic pancreatitis is a long-standing pancreas inflammation that results in permanent damage. It often develops after repeated episodes of acute pancreatitis or due to risk factors such as:
- Excess use of alcohol
- Smoking
- Genetic conditions (e.g., cystic fibrosis)
- Autoimmune diseases
- Pancreatic duct obstruction
- Elevated triglyceride or calcium levels
Three main components of chronic pancreatitis :
1. Persistent pain ( Due to duct narrowing or complications)
2. Enzyme deficiency
- Oily, foul-smelling stools (Steatorrhea)
- Unintentional weight loss
- Malabsorption of nutrients
3. Insulin-dependent diabetes
The role of intervention in chronic pancreatitis is just to relieve pain or complications.
Why is surgery needed?
While initial treatment includes medications, dietary changes, enzyme therapy and endoscopic treatment, some patients do not find sufficient relief. Surgery is typically considered in the following scenarios:
- Uncontrolled pain:
The most common reason for surgery is severe, persistent abdominal pain that significantly interferes with daily life despite medical treatment.
- Blocked pancreatic duct:
Scarring and inflammation can block the pancreatic duct, leading to pressure build-up and worsening symptoms.
- Pseudocysts or fluid collections:
Surgery may be necessary to drain or remove pseudocysts—fluid-filled sacs that can cause pain, become infected or compress nearby structures.
- Suspicion of cancer:
Chronic inflammation can sometimes mimic pancreatic tumours. When cancer is suspected, surgical intervention may be required both to establish a definitive diagnosis and to begin timely treatment.
- Severe structural damage:
When extensive damage occurs in parts of the pancreas, surgery may help restore digestive function and prevent further complications.
Types of surgery for chronic pancreatitis:
The choice of surgery depends on the patient’s symptoms, imaging findings, and overall health. Surgical procedures include:
1. Pancreatitis head coring with ductal decompression by lateral Pancreatico-jejunostomy (Frey’s Procedure)
- Ideal for: Patients with a dilated pancreatic duct
- Procedure: The pancreatic duct is surgically connected to the small intestine to allow drainage.
- Goal: Relieve pressure and improve pain management
2. Pancreatic resection
- Procedure: Removal of the damaged portion of the pancreas
- Types include:
- Distal pancreatectomy – Removes the body and tail of the pancreas.
- Whipple procedure (Pancreaticoduodenectomy) – Removes the head of the pancreas, part of the small intestine, bile duct, and gallbladder.
- Indication: When the disease is localised or when cancer is suspected.
Preoperative evaluation:
Before surgery, patients undergo a comprehensive evaluation that may include:
- Imaging: CT scan, MRI, or endoscopic ultrasound
- Blood tests: Pancreatic enzymes, blood sugar, liver function
- Nutritional assessment
- Pain management review
- Diabetes risk analysis
A multidisciplinary team — including gastroenterologists, surgeons, pain management specialists, endocrinologists, and dietitians, works together seamlessly to craft a personalised and comprehensive treatment plan.
Recovery after surgery:
Recovery varies depending on the procedure but generally includes:
Hospital stay:
- From 7 to 14 days
- Monitoring for pain, infection, and complications
Diet and digestion:
- Gradual reintroduction from liquids to solid foods
- Most patients require pancreatic enzyme supplements
- A low-fat, high-protein diet is typically recommended
Blood sugar monitoring:
- Insulin therapy may become necessary if the insulin-producing cells are lost or surgically removed.
- Close blood sugar monitoring and dietary adjustments are essential.
Long-term medication:
- Enzyme replacements for digestion
- Insulin or oral medicines for blood sugar control
Risks and complications:
As with any major surgery, there are potential risks, including:
- Bleeding or infection
- Leakage from surgical connections
- Delayed gastric emptying (slowed stomach emptying)
- Severe diabetic condition
- Nutritional deficiencies
- Dependence on enzyme or insulin therapy
Life after surgery:
Life after surgery requires adjustment but is manageable with the proper support. Key tips include:
- Take enzyme supplements with every meal
- Monitor blood sugar levels regularly
- Follow a nutritious, pancreas-friendly diet
- Avoid alcohol and smoking
- Attend regular follow-up appointments
Best gastroenterology department in Gujarat with expert digestive care.
In a nutshell :
Chronic pancreatitis can be both physically and emotionally exhausting. When conservative treatments are no longer effective, surgical intervention may provide much-needed relief and restore quality of life.
At KD Hospital, patients receive care from highly skilled gastroenterologists/gastrosurgeons in Gujarat. Our state-of-the-art facilities and personalised treatment plans ensure the highest standards of patient care and outcomes.