A LIVER TRANPLANT: REMOVE YOUR DISEASED OR INJURED LIVER (RIGHT) AND REPLACE IT WITH A HEALTHY LIVER (LEFT).
A liver transplant is a life-saving surgical procedure in which a diseased or injured liver is removed and replaced with a healthy liver. When medical treatments such as medications, endoscopy, or IV therapies are no longer effective, liver transplantation becomes the best option for survival.
Patients and families are usually offered two types of liver transplant options
Understanding the differences between DDLT and LDLT is crucial for making an informed decision that best suits the patient’s medical condition and personal circumstances.
Liver transplantation decisions can significantly impact
Although the transplant team makes the final decision, being well-informed allows patients and their families to understand their options and participate meaningfully in choosing the best outcomes.
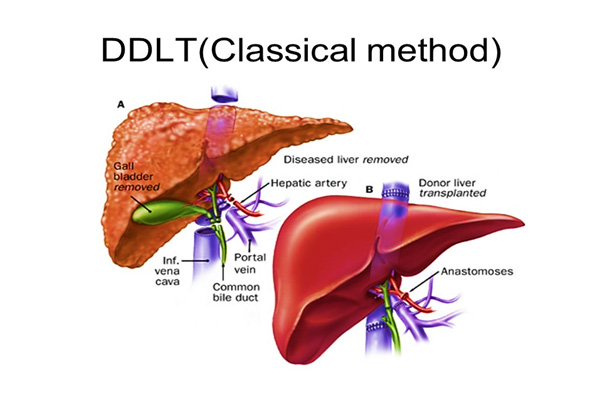
Deceased donor liver transplantation (DDLT) involves transplanting a whole liver from a brain-dead donor whose heart is still functioning. After obtaining consent from the donor’s family, the liver is retrieved and transplanted into a recipient with end-stage liver disease.
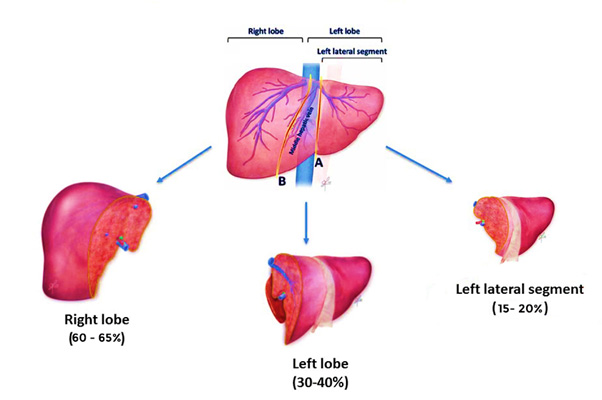
Living donor liver transplantation (LDLT) involves transplanting a portion of the liver from a healthy living donor, usually a close family member such as a parent, spouse, sibling, or child. Either the right or left lobe of the liver is donated.
The liver has a unique ability to regenerate. Within about three months, the donor’s and recipient’s livers undergo regeneration, restoring themselves to near-normal size and function.
| ASPECT | DDLT | LDLT |
| Donor source | Brain-dead donor (stranger) | Living family member |
| Liver size | Full liver transplanted | Partial liver transplanted (right/left lobe) |
| Timing | Dependent on donor availability (waiting period) | Planned, reducing waitlist mortality |
| Surgical risk | Standard liver surgery | Technically more complex, longer surgery |
1. Timely transplant
Surgery can be scheduled early, preventing deterioration of the patient’s condition.
2. Reduced waiting list mortality
Especially beneficial in regions where deceased donor organs are scarce.
3. Ideal for liver cancer patients
Patients with hepatocellular carcinoma (HCC) often have low MELD scores and may not receive a deceased donor organ in time.
4. Preferred option for paediatric liver transplant
The liver size can be tailored to fit infants and children.
Technically complex surgery
LDLT is more challenging and requires highly experienced transplant surgeons.
Risk to the donor
Although minimal, donors face surgical risks such as infection, bleeding, or bile leaks.
High waiting list mortality
Patients may worsen or die while waiting for an organ.
Higher overall cost
DDLT is generally more expensive than LDLT.
Risk of infection transmission
Limited evaluation time for deceased donor organs may increase infection risk.
During organ transport, insulated medical coolers play a critical role in preserving the donor liver. These coolers
The liver is placed inside the insulated container with ice packs to ensure viability until transplantation.
Choosing between DDLT and LDLT
Both DDLT and LDLT are proven, life-saving liver transplant options.
The best choice depends on:
At KD Hospital, the dedicated Liver Transplant Team combines advanced technology, multidisciplinary expertise, and streamlined clinical protocols to ensure high efficiency, safety, and optimal patient outcomes in both DDLT and LDLT procedures.
Always consult a qualified liver transplant specialist to determine the most appropriate option.
